Environmental monitoring is a fundamental element in maintaining controlled conditions within pharmaceutical manufacturing areas. By systematically collecting data on microbial and particulate levels in the air, on surfaces, and from personnel, it enables early detection of potential contamination and supports informed decision-making.
As part of the broader Contamination Control Strategy (CCS), environmental and process monitoring in cleanrooms is essential for minimizing risks that could compromise product quality.
A well-designed cleanroom monitoring program ensures compliance with GMP standards, particularly EU Annex 1 and FDA requirements, while safeguarding the integrity of both sterile and non-sterile products.
This article outlines best practices for implementing and optimizing environmental monitoring programs in the pharmaceutical industry, offering insights into sampling methods, data trending, and regulatory expectations.
What Is Environmental Monitoring?
Environmental Monitoring (EM) refers to the systematic collection and analysis of data related to microbial and particulate contamination in pharmaceutical manufacturing environments.
Pharmaceutical cleanroom monitoring involves both viable and non-viable particle surveillance to ensure environments remain compliant with GMP classifications and sterile manufacturing requirements.
The goal of EM is to verify that cleanroom conditions consistently meet the required cleanliness classifications, thereby supporting aseptic processing or other critical manufacturing steps.
This monitoring provides real-time and historical insights into the manufacturing environment, allowing for the early detection of deviations and the implementation of corrective actions before product quality is compromised.
EM is a key component of Good Manufacturing Practice (GMP) and is mandated by major regulatory bodies, including the EMA (Annex 1), FDA (21 CFR Part 211), and ISO 14644. It serves not only as a compliance requirement but as a risk-based tool to maintain product safety, especially in sterile drug manufacturing.

Cleanroom Classifications and Zoning
Cleanrooms used in pharmaceutical manufacturing are classified based on the concentration of airborne particles. These classifications define the environmental standards necessary to minimize the risk of contamination during production processes, particularly in the manufacture of sterile products.
The most widely recognized classification systems are the EU GMP Grades A to D and the ISO 14644-1 cleanroom classes. Grade A (equivalent to ISO Class 5) represents the most critical environment, typically used for high-risk operations such as aseptic filling.
SEE MORE: Cleanroom Classifications in GMP
Grades B, C, and D correspond to decreasing levels of cleanliness, used for background environments and less critical manufacturing steps. For example, Grade B often serves as a background for aseptic activities in Grade A zones, while Grade D might be suitable for handling non-sterile products.
Proper zoning within cleanrooms, distinguishing between critical, controlled, and support areas, is essential for designing an effective environmental monitoring program. Each zone must be evaluated for its contamination risk, which then determines the monitoring frequency, sample locations, and required action limits.
Areas with higher risk, such as open product exposure or sterile filtration steps, demand more intensive monitoring.
Regulatory guidelines emphasize that cleanroom classification must not be viewed in isolation but integrated into a facility’s Contamination Control Strategy (CCS). Environmental monitoring data should support the classification status, confirming that the environment remains within the validated state and consistently meets the design intent of the area.
Sources of Microbial Contamination
Controlling microbial contamination in cleanrooms begins with understanding its sources. The following are the most common sources in pharmaceutical manufacturing environments:

Personnel
Humans are the single most significant source of contamination in cleanrooms. Even with proper gowning, personnel constantly shed microorganisms from skin, hair, and mucous membranes.
Activities like walking, talking, or reaching into critical zones can release viable particles into the environment. Strict gowning protocols, movement control, and regular monitoring of gloves and garments are essential.
Air
Microorganisms in the air are typically attached to dust particles or skin flakes. These airborne contaminants may remain suspended or settle onto surfaces and products, depending on airflow patterns and turbulence.
Inefficient HEPA filtration or poorly balanced airflows can increase this risk. Monitoring airborne microbial levels and ensuring proper HVAC design are key to controlling the spread.
SEE ALSO: Types of HEPA Filters in Pharma Industry
Surfaces
Surfaces—including equipment, walls, floors, and work areas—can become contaminated through direct contact with personnel or by deposition from the air. Without regular cleaning and disinfection, these surfaces can support microbial growth, particularly in hard-to-clean areas or around worn or poorly maintained equipment.
Water
Water used in pharmaceutical processes must be tightly controlled and monitored. Inadequately maintained water systems can facilitate the formation of biofilms, which harbor and protect microorganisms. Routine monitoring of water for microbial content, Total Organic Carbon (TOC), and endotoxins is necessary to minimize this risk.
Equipment and Materials
Any item entering the cleanroom, including tools, packaging, and raw materials, can be a potential source of contamination. Insufficient cleaning, sterilization, or transfer procedures can introduce microorganisms. Proper material handling and disinfection at entry points are essential parts of contamination control.
Cleanroom Environmental Monitoring Program
An environmental monitoring program should be designed to assess the cleanliness of cleanrooms, collect data, and examine trends to show the state of microbiological control. An effective environmental monitoring plan should be designed to determine the cleanliness of cleanrooms, collect data, and evaluate trends that demonstrate the state of microbial control.
The monitoring program should also assess the effectiveness of cleaning and sanitization programs, evaluate the performance of personnel and equipment, and provide information about environmental control.
It is essential to be aware of the limitations of monitoring, as the methods used may vary in terms of collection efficiency and the ability to detect specific microorganisms. Monitoring provides a snapshot of the cleanroom environment at a specific time, and trends over time are more critical than individual results.
The cleanroom environmental monitoring plan typically encompasses:
- Total Particle Monitoring: This involves scrutinizing the total particle count in the air, ensuring the environment remains within the designated cleanliness class.
- Viable Particle Monitoring: Focusing on microbial contamination, this aspect includes regular checks on both the environment and personnel, crucial for aseptic operations.
- Climate Control Monitoring: Keeping a close eye on temperature, humidity, and other environmental factors is essential to prevent conditions that could encourage microbial growth or affect product stability.
- Advanced Product Sterility (APS) Checks: For aseptically manufactured products, APS checks are crucial to ensure the highest levels of sterility throughout the manufacturing process.
Total Particle Monitoring
This component of the environmental monitoring program focuses on measuring airborne non-viable particles to verify that cleanroom classifications remain within defined limits. Regular particle monitoring supports contamination risk assessment and demonstrates compliance with Good Manufacturing Practice (GMP) and Annex 1 requirements.
- Objective: To collect data on airborne particulate matter and assess air cleanliness in critical manufacturing areas, helping to identify potential contamination sources before they impact product quality.
- Implementation: Total particle monitoring should be integrated into the overall cleanroom environmental monitoring strategy, alongside viable monitoring, to provide a comprehensive picture of cleanroom performance.
- Cleanroom Monitoring: According to EU GMP Annex 1, maximum allowable concentrations are specified for particles ≥0.5 µm and ≥5.0 µm per cubic meter across cleanroom Grades A, B, C, and D, both “at rest” and “in operation.”
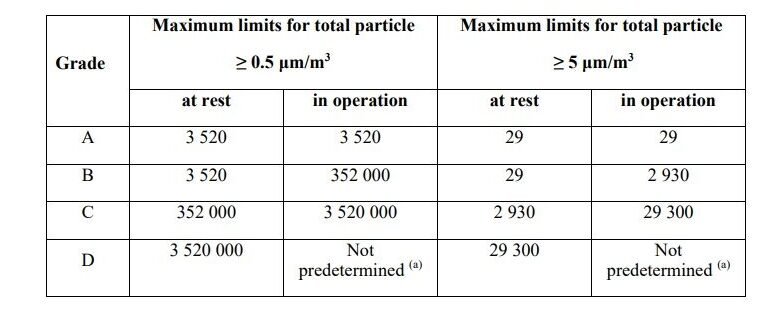
- Grade A Monitoring: Continuous particle monitoring is mandatory during all critical operations in Grade A areas, including the setup of equipment. A minimum sample flow rate of 28 liters per minute is recommended to ensure sufficient data capture.
- Grade B Monitoring: While not always requiring continuous monitoring analysis, Grade B areas should follow a similar approach with adjusted sampling frequency based on a documented risk assessment.
- System Selection: The choice of particle monitoring systems should reflect the specific risks of the manufacturing process, such as handling live organisms, powdery substances, or radiopharmaceuticals, and must not interfere with critical airflow patterns.
Viable Particle Monitoring
Viable particle monitoring targets the detection of living microorganisms in the cleanroom environment, including air, surfaces, equipment, and personnel. This type of monitoring is crucial for evaluating microbial control, particularly in aseptic processing areas where product exposure is most significant.
- Objective: To detect and quantify viable microorganisms in controlled environments, providing evidence that contamination risks are under control and aseptic conditions are maintained.
- Implementation: Monitoring should be conducted during routine operations, at the end of production, and during non-operational periods such as post-cleaning or before batch initiation. The frequency and method of sampling must be justified based on risk and regulatory expectations.
- Methods Used: A combination of settle plates, active air samplers, contact plates, and swabs is typically employed. Personnel monitoring includes sampling of gloves and gowns, especially during and after critical interventions. All methods should be validated and must not disrupt unidirectional airflow in Grade A zones.
- Monitoring During Operations: In Grade A and B areas, viable monitoring must be frequent and comprehensive. Monitoring should occur during processing, equipment assembly, and at defined intervals, with results trended over time to detect shifts in environmental control.
- Monitoring During Non-Operational Periods: Viable particle monitoring is also essential when cleanrooms are at rest. Sampling should be conducted after disinfection, before production startup, after batch completion, and following shutdowns to verify cleanroom recovery.

- Continuous Monitoring in Critical Areas: In Grade A areas, continuous viable air monitoring is required for the entire duration of critical operations. Grade B zones may adopt a similar approach, adjusted according to the risk to the aseptic process.
- Personnel Monitoring: Sampling frequency and locations should be defined by a risk assessment. Operators should be monitored during processes involving high contamination risks, with a focus on the integrity of gloves and gown surfaces. Methods should not interfere with the process or compromise product quality.
- Manual Operations Consideration: Where manual aseptic manipulations are performed, enhanced microbial monitoring of gowns and gloves is critical, given the higher potential for contamination.
Climate Control Monitoring
Monitoring environmental parameters, such as temperature, relative humidity, and differential pressure, is essential for maintaining the required conditions in pharmaceutical cleanrooms. These physical parameters directly influence air quality, microbial growth, and the overall stability of the manufacturing environment.
- Objective: To ensure that the cleanroom environment remains within predefined and validated limits, minimizing the risk of microbial proliferation and supporting product quality and stability.
- Parameters Monitored:
- Temperature and Humidity: Elevated humidity levels can promote microbial growth, while temperature deviations may affect product stability and personnel comfort.
- Differential Pressure: Ensures appropriate air movement between classified zones, preventing cross-contamination. Pressure cascades must be monitored continuously, particularly between Grade A/B and background areas.
- Implementation: Sensors and automated systems should be installed to provide real-time monitoring, with alarms triggered when values exceed alert or action limits. All data should be logged, trended, and reviewed regularly as part of the environmental monitoring program.
- Regulatory Expectations: EU GMP Annex 1 and ISO 14644 emphasize the importance of controlling and monitoring environmental conditions to ensure a stable and controlled environment. Any deviation from validated parameters must be investigated, with corrective actions implemented and documented.
- Integration with CCS: Climate control monitoring is a key part of the Contamination Control Strategy. It ensures that physical conditions do not compromise the microbiological state of control or interfere with critical operations.
Aseptic Process Simulation (APS)
Aseptic Process Simulation (APS), also known as a media fill, is a critical verification tool used to evaluate the effectiveness of aseptic process controls. It simulates the full aseptic manufacturing process using a sterile growth medium instead of the actual product, under conditions that closely mirror routine operations.
- Objective: To demonstrate that the aseptic process can consistently produce sterile products without contamination. APS validates operator practices, environmental controls, material transfer, and equipment handling under worst-case conditions.
- Process Design: The APS should replicate all critical aspects of the aseptic process, including:
- Equipment setup and sterilization
- Aseptic connections and interventions
- Container filling and sealing
- Duration and complexity of operations
- Personnel involvement and routine shifts
- The simulation must represent the maximum permitted batch size and run time, incorporating all critical interventions and potential risk scenarios.
- Media Selection: A nutrient-rich sterile growth medium, such as Tryptic Soy Broth (TSB), is typically used. The selected media must be capable of supporting a broad range of microorganisms to ensure reliable detection of contamination.
- Incubation and Inspection: After the simulation, filled units are incubated under validated conditions that promote microbial growth. All units are visually inspected for turbidity or other signs of contamination. Incubation typically occurs at two temperatures (20–25°C and 30–35°C) over 14 days.
- Acceptance Criteria: The goal is zero growth. Any contaminated unit is considered a failure and requires a comprehensive investigation to identify the root cause. Based on findings, corrective actions must be implemented and the simulation repeated to demonstrate regained process control.
- Frequency: APS should be performed:
- During initial aseptic process validation
- After significant changes to the process, equipment, or cleanroom layout
- Routinely, typically semi-annually for each aseptic line and operator qualification
Sampling Methods in Environmental Monitoring
Viable environmental monitoring involves the detection and enumeration of microorganisms present in cleanroom environments. Several sampling methods are employed to assess microbial contamination in air, on surfaces, and from personnel.
Each method has its own strengths and limitations, and their selection depends on the specific objectives of the monitoring plan and the sources of potential contamination.
Active Air-Sampling
Active air sampling quantifies viable microorganisms in a specific volume of air using mechanical air samplers. These devices typically use:
- Impaction samplers, which pull air through a perforated head, impacting microorganisms onto an agar surface.
- Centrifugal samplers, which swirl air inside a chamber, forcing microorganisms onto the agar by centrifugal force.
Passive Air-Sampling (Settle Plates)
Passive air sampling involves exposing agar settle plates to the environment to collect microorganisms that naturally settle by gravity. This method is:
- Simple, cost-effective, and easy to implement
- Useful for monitoring over longer periods without disrupting operations
Surface Sampling (Contact Plates and Swabs)
Surface sampling is used to evaluate the cleanliness of equipment and facility surfaces:
- Contact plates: Agar surfaces pressed directly against flat areas; offer high recovery but are limited to accessible surfaces.
- Swabs: Used for irregular or hard-to-reach areas where contact plates cannot be applied.
Personnel Sampling and Contamination Risk in Aseptic Processing
Personnel monitoring is critical in aseptic areas and assesses the microbial load on gloves, gowns, and garments:
- Finger plates: Detect contamination on gloved fingertips
- Gown plates: Assess microbial burden on gowns, sleeves, and other protective clothing
- Isolator/RABS sampling: Includes gloveports, gauntlets, and other critical barrier elements
Sampling Strategy and Frequency
A scientifically sound sampling strategy is fundamental to any cleanroom environmental monitoring (EM) program in pharmaceutical manufacturing. The strategy must not only fulfill regulatory expectations but also support continuous assurance of environmental control.
It should define what to sample, where, how often, and with which methods, tailored to the cleanroom’s function and contamination risk profile. The sampling strategy should be clearly defined in the site’s environmental monitoring protocol, detailing procedures for sample collection, locations, frequencies, and alert/action limit responses.
The basis of the strategy lies in applying contamination control principles to ensure that monitoring is representative, risk-based, and capable of detecting emerging issues before they affect product quality.
Risk-Based Approach to Sampling

Regulatory guidelines such as EU GMP Annex 1 (2022) emphasize the importance of risk-based EM planning. The selection of sampling points must be justified by a documented risk assessment that evaluates:
- Proximity to critical operations, such as aseptic filling, sterile filtration, or open container handling.
- Human intervention frequency, including manual manipulations and material transfers.
- Airflow patterns, especially in unidirectional airflow (UDAF) zones, where disruptions can lead to turbulence and particle redistribution.
- Historical contamination trends, using data to reinforce areas of concern or justify reduced frequency in low-risk zones.
- Design limitations and equipment layout, particularly in areas with potential dead zones, limited cleaning access, or equipment buildup points.
Risk-based mapping should include rationale for omitting any areas considered “low risk,” with periodic review to ensure assumptions remain valid.
SEE ALSO: Quality Risk Management (QRM)
Campaign-Based vs. Continuous Environmental Monitoring
Monitoring strategies must reflect the operational and microbiological risks associated with specific cleanroom zones and manufacturing steps.

Campaign-based Monitoring
It is typically applied in Grade C and D areas, where the likelihood of direct product exposure is lower. Sampling is performed at defined intervals during and after operations, which is often sufficient for trending and compliance purposes.
Continuous Monitoring
It is required in Grade A zones and expected in high-risk Grade B environments, especially during aseptic manipulations. For non-viable particles, real-time counters must operate continuously throughout processing, setup, and interventions.
For viable particles, continuous monitoring may not always be feasible; however, it should be as close to real-time as technology and process limitations allow.
Continuous monitoring analysis in the pharmaceutical industry ensures that contamination events are captured as they occur, rather than being missed between sampling intervals, which is critical for aseptic assurance.
Qualification of Sampling Points (Worst-Case Rationale)
Sampling points must be qualified based on worst-case positioning, locations most likely to detect contamination if control measures fail.
Qualification typically includes:
- Airflow visualization (smoke studies) to confirm airflow patterns, identify turbulence or air stagnation, and verify protection of critical zones.
- Simulations of personnel activity, to assess movement patterns and intervention hotspots.
- Proximity to critical control points (CCPs), such as product exposure stages or sterile connections.
- Assessment of recovery rate for viable sampling methods, ensuring that selected locations yield reliable results.
Documentation should include a justification matrix and layout diagrams. Requalification is necessary after equipment moves, process changes, or any event that alters the cleanroom environment.
Locations for Cleanroom Environmental Monitoring
Effective environmental monitoring depends not only on frequency and method, but also on the strategic selection of locations that reflect actual contamination risk. These should be aligned with contamination control strategy (CCS), facility zoning, and process mapping.
High-Risk Monitoring Locations
High-risk locations include, but are not limited to:
- Filling lines, open vessels, stopper bowls – where sterile products are directly exposed
- Material and personnel airlocks – especially during door transitions and material transfer
- Pass boxes and transfer hatches – transitional spaces prone to airflow disruption
- Areas near HEPA filters and air returns – potential points of contamination buildup or failure
- Manual intervention zones – where glove, gown, and human motion elevate contamination risk
Monitoring here helps confirm the integrity of critical control points and the surrounding environment.
Product Contact and Equipment Surfaces
Monitoring of product-contact surfaces and sterile equipment is vital to confirm that cleaning, sterilization, and setup processes are effective. Routine sampling of these surfaces should occur:
- After cleaning and before use
- After critical interventions or setup changes
- Post-operation, particularly in areas that contact sterile product or packaging components
Personnel-Intensive Areas
Personnel are the most significant source of contamination. Areas with high human activity require more frequent GMP monitoring:
- Gowning rooms and transfer zones
- Manual filling or compounding stations
- Operator workstations in Grade B backgrounds
Personnel monitoring (gloves, gowns, forearms) should be linked with these zones to assess contamination risk at its source.
Aligning Locations with Risk Assessments
Location selection should reflect the outcome of formal risk assessments, such as:
- FMEA (Failure Mode and Effects Analysis)
- HACCP (Hazard Analysis and Critical Control Points)
- Zonal risk mapping, supported by process flow and HVAC data
Monitoring locations should not be static; reassessment should occur when facility layouts change, product types shift, or trend data suggests an emerging risk.
Alert and Action Levels

In the context of environmental monitoring for pharmaceutical cleanrooms, setting appropriate alert and action limits is crucial for maintaining the required cleanliness standards and ensuring product safety.
These limits are predefined points that trigger a response when exceeded, indicating a potential shift away from normal operating conditions. The process of setting these limits involves a careful balance between regulatory requirements, historical data, and risk assessment.
Definition of Alert and Action Limits
Alert Limits: These are set to signal a level of environmental control that, while still within acceptable operational parameters, is approaching an unacceptable condition. When an alert limit is exceeded, it prompts increased scrutiny and potential preliminary investigation but may not require immediate corrective action.
Action Limits: These are set at levels where product quality, safety, or environmental control are potentially compromised. Exceeding an action limit necessitates immediate investigation and corrective actions to bring the environment back under control.
Establishing Limits Based on Regulatory Guidelines and Standards
Compliance with Standards: Alert and action limits should comply with relevant regulatory guidelines (e.g., FDA, EMA) and industry standards (e.g., ISO classifications for cleanrooms).
Reference to Industry Benchmarks: Standards and guidelines provide baseline values for microbial and particulate levels in different cleanroom grades.
Utilizing Historical Data and Trend Analysis
Data-Driven Approach: Historical environmental monitoring data from the specific cleanroom is invaluable for setting realistic and effective limits. This data helps in understanding the usual environmental fluctuations and identifying atypical variations.
Trend Analysis: Regular analysis of historical data helps in adjusting limits based on the actual operating conditions and trends observed over time.
Risk Assessment and Product Sensitivity
Risk-Based Setting: The nature of the product being manufactured and its sensitivity to contamination play a key role in setting these limits. More sensitive products may require more stringent limits.
Process Criticality: Areas or processes that are critical to product quality or more susceptible to contamination should have tighter limits.
Microorganism Identification and Trending
Identifying microorganisms recovered during environmental monitoring is essential for assessing contamination risk, especially in aseptic areas. In Grade A and B zones, species-level identification is expected to evaluate the potential impact on product quality and identify sources of contamination.
For Grade C and D areas, identification can be selective, based on elevated CFU counts, unusual colony morphology, or recurrence in trends. Any isolates linked to critical zones or post-intervention samples should be prioritized.
Using Identification for Control
Identification helps distinguish between random contamination (e.g. skin flora from personnel) and problematic trends (e.g. persistent environmental strains or waterborne organisms). Tracking the same species over time may signal ineffective cleaning or poor facility design.
Microbial Trending
Trending is a regulatory expectation and a practical tool. It provides visibility into the performance of your contamination control strategy over time.
Key trending practices include:
- Tracking by cleanroom zone, shift, and personnel
- Mapping recurring species
- Comparing trends across months or seasons
- Linking trends to interventions or process changes
When reviewed regularly, these trends support early detection of control issues and allow for targeted corrective actions.
Data Evaluation and CAPA Integration
Environmental monitoring data should not be viewed in isolation. A robust evaluation process is crucial for detecting patterns, assessing risks, and driving continual improvement. This involves not only reviewing individual results but also interpreting data across time, locations, and process conditions.
Routine data evaluation should include:
- Trend analysis for each cleanroom grade and sampling location
- Review of personnel and process-associated contamination
- Comparison of shifts, campaigns, and interventions
- Assessment of alert and action limit breaches
All findings must feed directly into the site’s Corrective and Preventive Action (CAPA) system.
When limits are exceeded or unusual trends emerge, a structured investigation must follow. This includes identifying the root cause, evaluating product impact, and implementing measures to restore control.
CAPAs may involve retraining personnel, modifying cleaning procedures, revising gowning protocols, or reassessing airflow design and sampling strategy.
The integration of EM data with deviation systems ensures that environmental risks are actively managed and that the contamination control strategy remains effective over time.
Regulatory Guidelines for Environmental Monitoring
Environmental monitoring is a core GMP requirement and is regulated through several internationally recognized guidelines. These documents outline expectations for cleanroom classification, sampling strategies, data evaluation, and contamination control.
GMP environmental monitoring requirements, outlined in EU Annex 1 and FDA 21 CFR Part 211, emphasize a risk-based, documented approach to monitoring cleanroom conditions in GMP-compliant facilities.
EU GMP Annex 1 (2022 Revision)
- Emphasizes a risk-based approach and integration into the Contamination Control Strategy (CCS)
- Requires documented rationale for sampling frequency, methods, and locations
- Specifies microbial and particulate limits for cleanroom Grades A to D
- Mandates continuous particle monitoring in Grade A zones and routine trending of data
- Stresses the importance of root cause investigations and CAPA implementation
FDA 21 CFR Part 211
- Requires control over environmental conditions to prevent microbial and particulate contamination
- Mandates investigation of any non-conformance, including EM excursions
- Cleanroom conditions must be appropriate for the intended use and maintained throughout production
ISO 14644-1 and ISO 14644-2
- Define standards for cleanroom classification and routine particle monitoring
- Provide guidance for qualification, monitoring intervals, and limits for non-viable particles
FAQ
How Often Should Environmental Monitoring be Conducted in Cleanrooms?
The frequency of environmental monitoring depends on several factors, including the cleanroom grade, the type of manufacturing process, and regulatory guidelines. It typically ranges from continuous monitoring in critical areas to periodic checks in less critical zones.
How are Viable Particle Monitoring Results Interpreted?
Viable particle monitoring results are interpreted based on established alert and action limits. Trends and deviations from normal patterns are more critical than individual results.
How Is the Recovery Efficiency of Environmental Monitoring Methods Validated?
Recovery efficiency is validated through method qualification studies using known quantities of microorganisms or particles introduced onto surfaces or into the air. Each environmental monitoring method must demonstrate acceptable recovery rates under actual or simulated cleanroom conditions to ensure reliability in detecting contamination.
How Is Cleanroom Behavior of Operators Monitored and Linked With EM Data?
Operator behavior is monitored through direct observation, routine personnel sampling (e.g., gloves, gowns), and correlation of EM excursions with intervention logs.
What Role Does Disinfectant Efficacy Testing Play in Interpreting Environmental Monitoring Trends?
Disinfectant testing ensures that cleaning agents effectively eliminate common environmental isolates. If elevated counts persist, it may indicate reduced efficacy, prompting requalification or a review of cleaning frequency and rotation.
How Are Environmental Isolates Used to Challenge Media During Growth Promotion Testing (GPT)?
Recovered isolates are used to confirm that the growth media supports the growth of organisms present in the facility. Including these strains in GPT ensures that the detection system remains sensitive to relevant contaminants.
What Sampling Practices Are Recommended When Using Isolators or RABS in Aseptic Environments?
Sampling should target gloveports, internal surfaces, and surrounding air without breaching containment. Closed-loop systems and sterile sampling tools are essential to maintain sterility during routine monitoring and interventions.
How Often Should Laboratory Environmental Monitoring Be Conducted?
The monitoring frequency is based on risk assessment, laboratory classification, and the type of activity. For microbiological labs or those handling sterile samples, laboratory environmental monitoring may be performed daily or on a shift basis, while other labs may follow a weekly or campaign-based schedule.
Final Thoughts
Environmental monitoring is a critical component of maintaining cleanliness and microbiological control in pharmaceutical manufacturing environments. By implementing an effective environmental monitoring program, pharmaceutical companies can identify potential sources of contamination, assess the effectiveness of cleaning and sanitization programs, and ensure the control of cleanroom environments.
Ultimately, the purpose of environmental monitoring in pharmaceutical industry operations is to ensure microbiological control, support GMP compliance, and protect product quality throughout the manufacturing lifecycle.